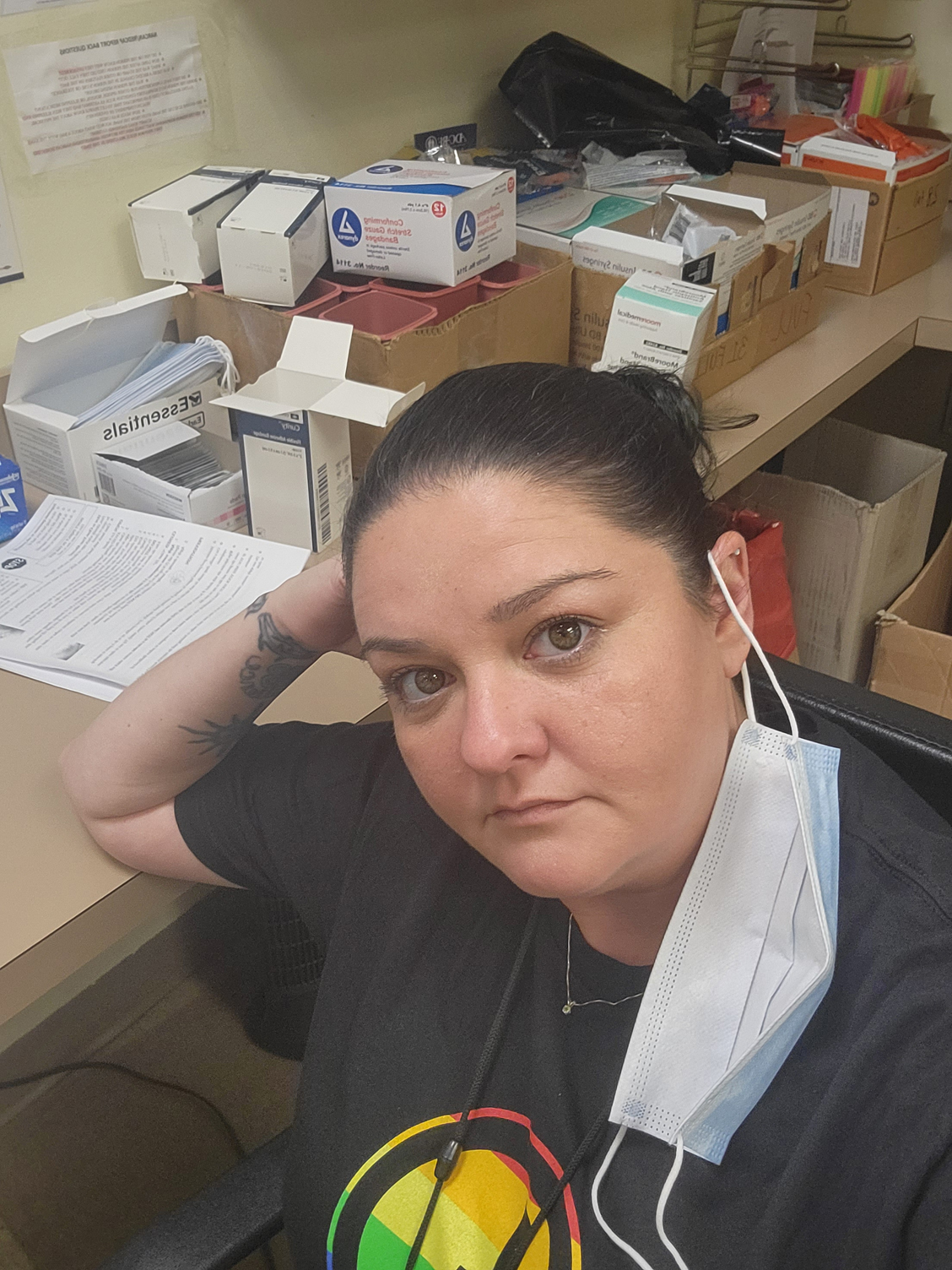
Service Provider Works in Hard-Hit Area
By Luke Schmaltz, VOICES Newsletter Editor
“Some of our finest work comes through service to others.” – Gordon B. Hinckley
For the last two years, Erika Hensel has been working in Holyoke and Springfield, assisting people in the alleys and encampments who are struggling with substance use. On any given day, she could be found distributing harm reduction materials, applying wound care, and offering kind words to individuals in need. “I would be where people are actively using drugs, helping them get clean syringes … and naloxone,” she explains.
Direct Engagement
As the former Overdose Engagement Coordinator for Tapestry Health, Hensel witnessed the negative results of substance use through the most up-close and personal lens possible. “A lot of things happen in the alleys, especially where people are using drugs — a lot of overdoses, a lot of deaths. I engaged with a lot of the sex workers in Holyoke, and the violence towards them is unimaginable,” she says. “Holyoke is an open-air drug market, full of trap houses where you can buy anything – including people.”
A Real-Life Nightmare
Hensel describes the scene along a section of Elm Street, one of the town’s main thoroughfares, “In the alley behind Elm Street, even during the day, you’re seeing people lined up, actively injecting or smoking crack and engaged in different means to get money to do that. There were days when I’d walk into the alley and see 30 to 40 people on that stretch. It’s a pretty high-traffic area,” she explains.
“I’ve probably Narcanned at least 50 people,” Hensel continues. “I’ve had my best friend and my partner overdose in my home, and I didn’t think they were going to make it. The majority of my senior class is dead now from drugs. We started dying when I was in high school in the Marlborough/Hudson area. OxyContin hit huge, everybody was saying it was non-habit-forming, that it was safe, they prescribed it to everyone, there were commercials for it, you could buy it online, and then we had our first death. He was 17 and the first one of us to go. It was such a shock at the time, the idea that someone could die of pills. Now, every couple of months you get the call, or the Facebook post, and you become numb to it.”
“Doctors were getting kickbacks for prescribing these pills to people and it just blew up,” Hensel continues. “For a kid like me, who had a long list of addicts in her family in a town with not much to do, it was a lot to deal with.”
A Rare Survivor
Hensel has been in recovery for the better part of the last decade, after living through the OxyContin wave. “There was a real seriousness to what we were doing,” she reflects, “especially since Oxy was looked at like Percocet, not as a ‘real’ drug. There was no D.A.R.E. class for prescription pills. Death from overdose wasn’t just something that happened to other people, it could happen to you, it could happen to anyone,” she says.
In November 2022, Hensel accepted a position as Community Coordinator with the HEALing Communities Study, which is focused on reducing opioid use in Holyoke and Springfield. Yet, she reflects on her time at Tapestry Health with a sense of accomplishment. “I was pretty good at my job,” she begins. “It doesn’t matter to me if you haven’t showered in six months, you don’t have any social support, and you’re trespassing or if you’re a top businessman…everyone is just as valuable. I treat everyone genuinely and in doing so I tend to have a lot of people open up to me.”
Hensel explains how being a service provider places her in the role of confidant for grieving people. “You tend to have people open up about all kinds of things,” she says. “People tell me about the overdoses they have encountered, the deaths, their own suicidal thoughts and their struggles to try and put their lives back together. The job was handing out syringes and Narcan, but what it really was, was being a human connection for another person and connecting them with services or just listening and giving them peer support.”
The Importance of Self-Care
When it comes to her own mental health, Hensel admits her profession isn’t easy. The work can take a mental and physical toll, especially the collective grief that builds up after seeing people struggle and die on a daily basis. “You’re being traumatized damn near daily,” she begins. “I’ve found dead bodies, I’ve lost people, I’ve given CPR until my arms gave out trying to bring someone back and they’re not coming back.”
“You learn to put it in a box, and you don’t open the box because you’re just going to be paralyzed. I did that for the first couple of years in this profession. But at some point, the box becomes too big and you either burn out, you relapse, or you figure it out,” she explains.
Hensel adheres to a distinct regimen of self-care for dealing with the grief that accumulates in her profession. “A change of scenery really helps,” she says. “Also, peer support training through peer support organizations is really important. They really made me focus and realize that I’m not the end-all be-all and that there are so many people in this community who care and are willing to pick up the slack, that it’s not always on me, and that I deserve time and boundaries just like everyone else.”
“So that’s the next thing,” Hensel continues, “Setting up boundaries. I’m not going to pick up my phone after work, it doesn’t matter. You have to set those boundaries and stick to them. Also, if you’re in this profession, you have to go to counseling. You have to have someone who can be there to listen.
“When the trauma becomes so big, seeing people that I love die, Narcanning people that I love, programs like the SADOD peer grief programs really help. It makes you feel like you’re not alone. You share the grief, you voice it, you open the box a little bit and you’re letting it go. You’re not holding onto it anymore,” she explains.
“Also, doing things for yourself like going to the gym, getting my nails done, taking a nap – those things help too.”
Moving Forward
Hensel looks forward to her new role and the challenges that await. “Now, I’m on the other side,” she says. “I’m creating initiatives that are aimed at reducing overdoses by 40%. I was chosen by the Springfield community based on my experience and my ability to connect with people who are actively using drugs. I can bring their voices to the table to make the community decisions about what we know about Springfield, what we think would help Springfield, what people who are using need and then making it happen.”
Hensel’s new position carries distinction, yet she is quick to assert her humility. “It’s a big step up and I don’t even have a degree,” she says.
Regardless, most would agree that her hands-on experience and dedication carries more professional credibility than any college degree could possibly convey. “My heart is in those alleys and probably, after the study is concluded, I’ll be back there.” she says.